 Felicia Graham, a resource nurse at Highsmith-Rainey Specialty Hospital, has spent years caring for patients. In July 2023, she found herself in a new role — the patient.
Felicia Graham, a resource nurse at Highsmith-Rainey Specialty Hospital, has spent years caring for patients. In July 2023, she found herself in a new role — the patient.
At 42, she scheduled her first mammogram in late July, thinking it would be nothing more than another box checked on her annual physical. Instead, it became the start of a journey that would test her strength, faith and resilience.
The mammogram came back abnormal, leading to additional imaging and a biopsy. At first, doctors diagnosed her with stage one breast cancer. But magnetic resonance imaging (MRI) revealed something more serious — two tumors, each a different type of cancer, in separate locations. The cancer had reached her chest wall, elevating her diagnosis to stage three.
"The difference between stage one and stage three is huge," Graham explained. "Stage one is usually smaller tumors that can be removed with surgery. Stage three can be bigger, more aggressive and sometimes spread. Mine hadn’t reached my lymph nodes, but because of its size and location, the treatment plan had to change."
Instead of heading straight into surgery, her care team decided to start with chemotherapy to shrink the tumors before operating. Graham underwent 20 rounds of chemo over six months; four rounds of AC (adriamycin and cyclophosphamide), a common chemotherapy regimen; followed by 12 rounds of Taxol, another intravenous (IV) infusion.
"It was rough, but I managed," she said. "I was tired and weak, but I didn’t have the extreme side effects some people experience. I stayed as positive as I could."
On March 5, 2024, Graham had a bilateral mastectomy. Initially, her surgeons hoped to preserve her nipples, but tissue testing showed traces of cancer remained. For several months, she lived with the mental weight of knowing her battle wasn’t fully over. In August, she underwent a second surgery, this time with complete reconstruction and the relief of hearing she was finally cancer-free.
The experience transformed more than just her health; it changed her entire outlook on life.
"The journey through fighting cancer has changed my whole lifestyle," Graham said. "It changes the way I eat, the way I exercise, the way I live my life, the way I spend my time. Getting back to work was a big thing for me because it gave me the opportunity to take care of people again. Now I have the voice to say, ‘Hey, I’ve been the patient. I know what it’s like to be there.’"
She says the positives she’s gained from such a difficult experience will stay with her forever. "Life is changed in abundance for me, because I look at everything differently. Time has more value. Family has more value. Being able to do my job and care for patients has more value. I want people to know there are people who care, people who understand, and we’re here for them, just like the people who cared for me."
Her care began at Cape Fear Valley Health Pavilion North’s Cancer Center with oncologist Dr. Matthew Carpenco, who oversaw most of her treatment. She also worked closely with surgeon Dr. Hall, who first explained her stage three diagnosis, general surgeon Dr. Elizabeth Sawyer, and plastic surgeon Dr. Leif Nordberg, who continues to monitor her recovery.
"I absolutely would recommend Cape Fear Valley," Graham said. "From the very beginning, they were on top of everything. Within 24 hours of my mammogram, I was called back for a second look. Days later, I had my biopsy. Dr. Pink made sure I had a PET scan, an MRI — everything to cover the ground. Every single person I encountered was great. They really took care and supported me, both as an employee and as a patient."
Today, Graham says she feels amazing, physically stronger, mentally tougher and more determined to live fully. While she still manages some side effects from treatment, she’s found ways to take care of herself holistically and share what she’s learned with others.
“My biggest thing now is encouraging people to get tested,” she said. “Breast cancer was not something that ran in my family. Had I not gone when I did, my story would have been absolutely different. Early detection is the best thing you can do for yourself. Don’t wait; make the appointment, check yourself and take care of yourself. And yes, that goes for men too.”
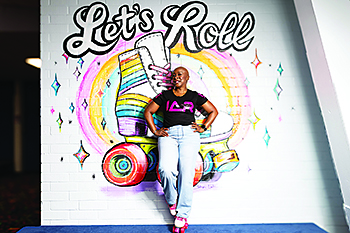
(Photo courtesy of Cape Fear Valley Health)