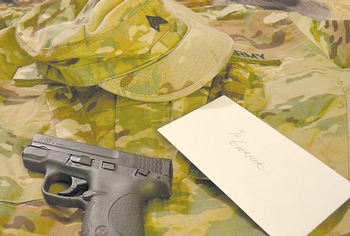
 America is facing a national public health crisis. Each day, 22 veterans, service members, reservists and members of the National Guard die by suicide, totaling more than 7,300 deaths per year. Three veterans shot and killed themselves at Veterans Affairs facilities within five days late last month. While Veterans Affairs has been the public face of the issue, veterans are in many ways an amplification of the same factors that drive suicide in the broader American population: a shortage of mental health resources, a lack of funding for suicide research, and easy access to guns, according to the VA National Suicide Data Report.
America is facing a national public health crisis. Each day, 22 veterans, service members, reservists and members of the National Guard die by suicide, totaling more than 7,300 deaths per year. Three veterans shot and killed themselves at Veterans Affairs facilities within five days late last month. While Veterans Affairs has been the public face of the issue, veterans are in many ways an amplification of the same factors that drive suicide in the broader American population: a shortage of mental health resources, a lack of funding for suicide research, and easy access to guns, according to the VA National Suicide Data Report.
The 2015 Clay Hunt Suicide Prevention for Americans Act requires officials to provide annual reviews of mental health care and suicide prevention programs. It found that veterans receive good mental health care at many Department of Veterans Affairs centers, but that has not decreased suicide rates. Some programs to address veteran suicide are showing promise. A relatively new program, known as the Mayor’s Challenge, helps city and state governments reach more veterans through public health programs via Veterans Affairs partnerships. Separately, former Fayetteville Mayor Nat Robertson collaborated with retired Fayetteville VA Medical Center Director Elizabeth Goolsby to launch a local outreach challenge on veterans’ needs.
A study of nine VA emergency rooms found 45 percent fewer suicidal behaviors among patients who received follow-up outreach after suicide attempts. As a result of this study, all VA medical centers have put in place a safety planning intervention program. Yet about 70 percent of veterans do not regularly use VA access to federal facilities that may be viewed as central to suicide prevention.
Exposure to combat is considered a leading cause of post-traumatic stress disorder among veterans. PTSD is a psychiatric condition in people who experienced or witnessed a traumatic event. “We need to expand our understanding of mental health among veterans,” said Rep. Mark Takano, DCalif., chairman of the House Veteran Affairs Committee. “We need to commit to providing the resources needed to implement a comprehensive plan.”
A 2014 Veterans Health Administration audit unearthed rampant problems, including allegations that scheduling delays led to 40 Arizona veterans dying from lack of timely medical care by the VA.
“Providing same-day 24/7 access to mental health crisis intervention and support for veterans, service members and their families is our top clinical priority,” said VA secretary Robert Wilkie in an April 16 press release. “It’s important that all Veterans, their family and friends know that help is easily available.”
Yet myriad political, structural and cultural impediments exist far beyond Washington, D.C. Many suicide experts believe that a lack of proper training in suicide prevention in the broader mental health field, hobbled by a lack of research, is central to the issue.
The VA’s Office of Mental Health and Suicide Prevention is a national leader in making high-quality mental health care and suicide prevention resources available to veterans through a full spectrum of outpatient, inpatient and mental health services. Veterans in crisis — or those concerned about one — should call the Veterans Crisis Line at 800-273-8255 and press 1, send a text message to 838255, or chat online at VeteransCrisisLine.net.